Have you ever felt stuck in your spine when moving, as if certain motions are just out of reach? This sensation can be frustrating and may indicate a lack of spinal mobility!
What is Spinal Mobility?
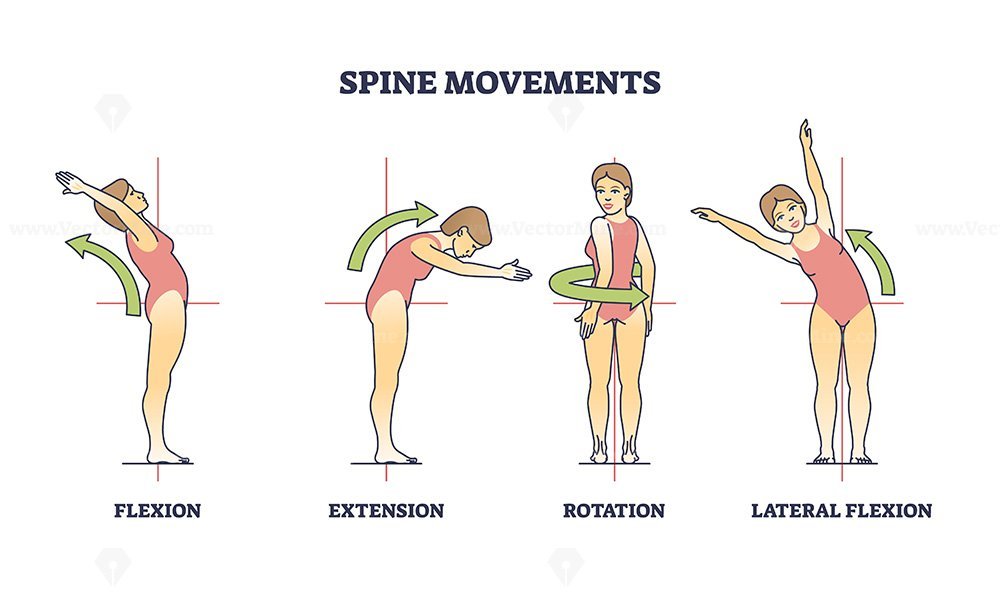
Spinal mobility refers to the ability of the spine to move freely and effectively through its natural range of motion. This encompasses several types of movements, including:
1. Flexion (bending forward)
2. Extension (bending backward)
3. Lateral flexion (bending to the sides)
4. Rotation (twisting movements)
Good spinal mobility is essential for maintaining overall physical health, as it allows for efficient movement during daily activities, sports, and exercise.
How’s Limited Spinal Mobility affecting body wellness:
Reduced spinal mobility can have several negative effects on overall health and well-being.
a. One of the most common issue is bringing pain and discomfort
b. Limited spine mobility also can lead to stiffness and chronic pain in the back, neck, and associated areas.
c. Additionally, reduced mobility often contributes to poor posture, which can result in further musculoskeletal problems and discomfort.
Therefore, spinal mobility is essential for maintaining a healthy, active lifestyle. A flexible spine can enhance your overall movement quality, reduce the risk of injury, and alleviate discomfort. Whether you’re an athlete or someone who spends long hours sitting at a desk, incorporating spinal mobility exercises into your routine can help alleviate tension and improve flexibility.
Physiotherapy can assist you in managing it
The good news is, women dealing with urinary incontinence can take comfort in the fact that physiotherapy can help!
We’d like to show how we can help:
- Pelvic Floor Exercises: Tailored exercises help strengthen weakened pelvic floor muscles. These exercises are discreet, easy to perform, and can be integrated into daily routines.
- Bladder Training: Physiotherapists guide women in developing a schedule for bathroom visits, gradually increasing the time between them. This helps retrain the bladder and improve control.
- Lifestyle Modifications: Managing fluid intake, maintaining a healthy weight, and avoiding bladder irritants, can significantly contribute to symptom improvement.
- Education and Support: Physiotherapists educate women about the anatomy and function of the pelvic floor, empowering them to actively participate in their treatment.
Physiotherapy can assist you in managing it

By incorporating targeted exercises, lifestyle adjustments, and expert guidance, women can regain control over their bladder function and enhance their overall quality of life. From postnatal recovery and pelvic health to musculoskeletal issues and beyond, physiotherapy plays a pivotal role in guiding women toward strength, resilience, and optimal functioning.
If you or someone you know is dealing with urinary incontinence, consider consulting a physiotherapist at Your Physio to embark on a journey towards improved pelvic health and quality of life.
Prepared by:
Vanessa Fong Poh Jing
Your Physio Kepong

